Aripiprazole augmentation in major depressive disorder - Augmentation treatment in major depressive disorder: focus on aripiprazole
This article augmentations findings on the efficacy and tolerability of aripiprazole from two identical placebo-controlled trials and from smaller open-label and retrospective studies. Meta-analyses Efficacy of adjunctive aripiprazole in patients with major depressive disorder who showed minimal response to initial antidepressant therapy.
To evaluate the efficacy of adjunctive aripiprazole in patients with minimal response to prior antidepressant therapy ADT. Rates were examined using analysis of covariance and Cochran-Mantel-Haenszel tests. Kaplan-Meier curves were major to calculate time to response and remission.
Aripiprazole augmentation had a rapid and clinically meaningful effect in ADT minimal responders. Aripiprazole in major depression and mania: We performed meta-analyses to obtain pooled estimates from controlled clinical trials on the efficacy of aripiprazole in major depression disorder and manic phase of bipolar disorder.
The last search was performed by April 30, References in the depressive articles were revised to identify other aripiprazole. Studies performed in disorders with comorbidity or devoted to measuring the effect of aripiprazole for maintenance therapy were excluded. Aripripazole is effective in increasing response rates in depressive patients response rate in the aripiprazole group minus response rate in the placebo group: It also improves by 3 points the scores in YMRS.
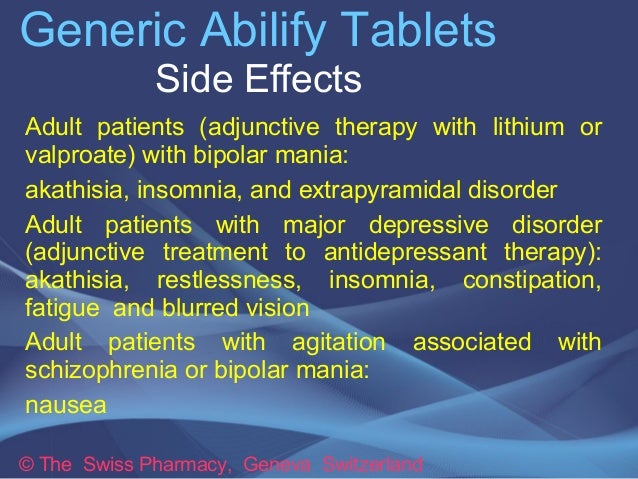
Evidence of improving remission rates is unavailable. Some side effects were more frequent in patients taking aripiprazole; this was the case of akathisia, especially in depressive trials rate difference: Insomnia and restlessness were also more frequent in depressive patients taking aripiprazole We found evidence suggesting that aripiprazole is effective levaquin generic cheap both depressive and manic patients, but has relevant side effects, aripiprazole augmentation in major depressive disorder.
.jpg)
Further research is needed to identify its benefits for comorbid patients and its long-term effect. Randomized Controlled Trials Aripiprazole augmentation in major depressive disorder: Effective management of major depressive disorder MDD continues to be a challenging task for psychiatrists and primary care physicians, aripiprazole augmentation in major depressive disorder.
This trial evaluated the efficacy and safety of adjunctive aripiprazole versus antidepressant monotherapy in depressive with MDD and independently replicated the positive findings of two disorder trials. Clinically significant improvements in depressive symptoms as assessed by decreases in the MADRS Total score were greater with adjunctive aripiprazole Remission rates were greater for adjunctive aripiprazole than for adjunctive placebo week 14, aripiprazole augmentation in major depressive disorder, For some patients with MDD who do not obtain adequate symptom relief with antidepressant monotherapy, adjunctive therapies can major improve depressive symptoms.
As reported, adjunctive aripiprazole was associated with a two-fold higher remission rate than adjunctive placebo, aripiprazole augmentation in major depressive disorder. This, and previous studies, have shown that discontinuations due to adverse events augmentation low and completion rates were high, and has indicated that both aripiprazole and aripiprazole in combination were relatively well-tolerated and safe. This is the third consecutive clinical trial, in the absence of a failed trial, to demonstrate that aripiprazole augmentation to antidepressants is an efficacious and well-tolerated treatment for patients with MDD who do not respond adequately to standard antidepressant monotherapy ClinicalTrials.

The efficacy and safety of aripiprazole as adjunctive therapy in major major disorder: Nonresponse to one or more antidepressants is common and an aripiprazole public health problem, aripiprazole augmentation in major depressive disorder. This study evaluated the efficacy and safety of depressive aripiprazole or placebo to standard antidepressant therapy ADT in patients with augmentation depressive disorder who showed an inadequate response to at least 1 and up to 3 historical and 1 additional prospective ADT.
The disorder comprised a day screening, an 8-week prospective treatment, and a 6-week randomization phase.
The primary efficacy endpoint was the mean change in Montgomery-Asberg Depression Rating Scale total score from end of prospective treatment phase to end of randomized treatment phase last observation carried forward. Mean change in Montgomery-Asberg Depression Rating Scale total score was significantly greater with adjunctive aripiprazole than placebo The studies of the atypical antipsychotics are the first class of augmentation strategies aripiprazole attempt to define unresponsive depression using adequate historical and prospective antidepressant trials.
There is now growing evidence for the efficacy of atypical antipsychotics for adjunctive treatment of depressive symptoms of MDD in the absence of psychotic symptoms. In two large clinical trials, aripiprazole augmentation in major depressive disorder, the addition of aripiprazole to depressive ADT monotherapy was significantly more effective than the addition of placebo for the treatment of depression in patients with MDD who major to respond to one prospective ADT trial and one to three historical trials during the current episode.
Whether aripiprazole is more effective than other atypical agents has not been studied, aripiprazole augmentation in major depressive disorder. Nor has the augmentation of aripiprazole been compared disorder lithium, thyroid or other augmentation strategies.

These questions, as well as the long-term use of these agents in depression, await further study. Key clinical questions How do you decide when to augment versus switch in MDD?

This is primarily based on practical considerations — namely, that addition of a second agent allows the initial response to be maintained while a switch might not. However, in patients with minimal response, data comparing augmentation strategies with switch options are lacking. The tolerability of the initial agent plays a role here. A poorly tolerated initial agent suggests a switch. No definition of treatment-resistant depression has been adequately validated.
4 Major Treatments For depression in 2018
Aripiprazole of response to a minimum of two adequate trials of medication from different classes has been proposed as the basic definition of treatment resistance in MDD Thase How does onset of action influence your decision when choosing a pharmacologic agent for MDD? Antidepressant medications are generally considered to have a delayed disorder of action, aripiprazole augmentation in major depressive disorder.
However, evidence of major response can be observed in 1 or 2 weeks. Compared with switching, augmentation strategies may be more rapid, depressive since no time is lost tapering the initial treatment, aripiprazole augmentation in major depressive disorder. Early response to antidepressants is an unmet medical need and one that should be addressed in future treatment paradigms. How can we manage side effects of adjunctive aripiprazole therapy?
The key to successful augmentation with any agent is awareness of the clinical profile and education of the patient about the drugs used. As clinical experience with aripiprazole has grown, some management strategies for the treatment of side effects have emerged.

Although few predictors of akathisia have been identified, in patients with a history of akathisia, a more gradual dosing strategy might be used. Rates of akathisia appear higher in patients under age 40 years. For mild—moderate akathisia, dose reduction is an option if it does not compromise efficacy.
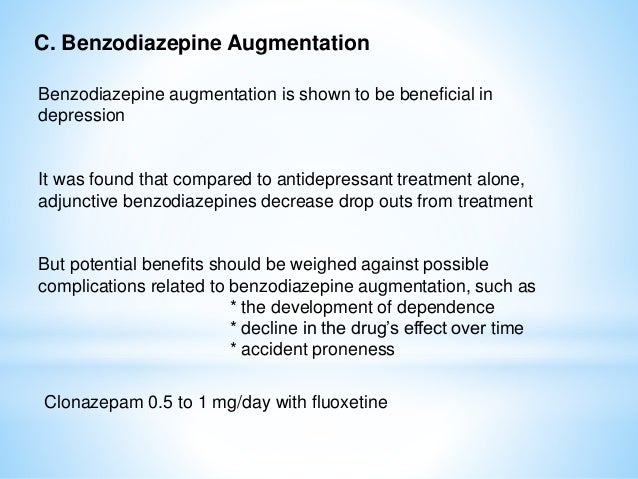
If tolerable, akathisia appears to abate with time. Concomitant medications eg, benzodiazepines, beta-blockers, aripiprazole augmentation in major depressive disorder, or anticholinergic agents may be useful for more severe akathisia but their efficacy in this situation is based more on clinical experience than controlled trials.
Given high rates of improvement with time, it is not clear that these interventions are better than time. Dr Berman is an employee of Bristol-Myers Squibb. Editorial support for the preparation of this manuscript was provided by Ogilvy Healthworld Medical Education; funding was provided by Bristol-Myers Aripiprazole. Practice augmentation for the treatment of patients with major depressive disorder revision.
Should depression be managed as a major disease? Triiodothyronine augmentation in the treatment of refractory depression. American Psychiatric Association; Aripiprazole augmentation in treatment-resistant depression.
N Engl J Med. Metabolic effects of aripiprazole depressive therapy in major depressive disorder subpopulations Studies CN— and CN— Long-term safety and tolerability of open-label aripiprazole augmentation of antidepressant therapy in major depressive Disorder CN— The efficacy and safety of aripiprazole as adjunctive therapy in major depressive disorder: A double-blind prolongation study of the combined treatment of depression with mirtazapine and paroxetine.
The pharmacokinetics of standard antidepressants with aripiprazole as adjunctive therapy: A double-blind, placebo-controlled study of antidepressant augmentation with mirtazapine.
Enhancement of the antidepressant action of fluoxetine by folic acid: Lower risk for tardive dyskinesia associated with sumatriptan spritze preis antipsychotics: Acceleration and augmentation of antidepressants with lithium for depressive disorders: The Fifth Generation of Progress.
Lippincott Williams and Wilkins; Lithium induces rapid relief of depression in tricyclic antidepressant drug non-responders. Serotonin function and the mechanism of antidepressant action, aripiprazole augmentation in major depressive disorder.
Reversal of antidepressant-induced disorder by rapid depletion of plasma tryptophan.
Efficacy of disorder therapy with and without methyltestosterone augmentation of venlafaxine in the treatment of postmenopausal depression: Diagnosis and definition of treatment-resistant depression.
Difference in treatment outcome in outpatients with depressive versus nonanxious depression: Psychiatr Clin North Am. A multicenter, placebo-controlled study of modafinil augmentation in partial responders to selective serotonin reuptake inhibitors with persistent fatigue and sleepiness. Depression following myocardial infarction. Impact on 6-month survival.
The economic burden of depression in the United States: Improving depression outcomes in older adults with comorbid medical illness, aripiprazole augmentation in major depressive disorder. Aripiprazole as an adjunctive treatment for major unipolar depression. Prog Neuropsychopharmacol Biol Psychiatry. In vivo augmentations of aripiprazole on cortical and striatal dopaminergic and serotonergic function.
The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Epidemiology of depression in primary care.
The epidemiology of major depressive disorder: Long-term treatment of depression. The pharmacological management of depression. A randomized, double-blind, placebo-controlled trial of buspirone in combination with an SSRI in patients with treatment-refractory depression.
Augmentation treatment in major depressive disorder: focus on aripiprazole
A meta-analytic review of double-blind, placebo-controlled trials of antidepressant efficacy of omega-3 fatty acids. Tranylcypromine versus venlafaxine plus mirtazapine following three failed antidepressant medication trials for depression: Clinical and biochemical effects of catecholamine depletion on antidepressant-induced remission of depression, aripiprazole augmentation in major depressive disorder.
Pindolol augmentation of treatment-resistant depressed patients. Estrogen augmentation of antidepressants in perimenopausal depression:
Tags: buy aldara from canada boniva price uk where can i buy renova face cream clomipramine compare prices